Frozen embryo transfer (FET) has become one of the most common and successful approaches in modern IVF treatment.
Unlike fresh embryo transfer, FET allows embryos to be cryopreserved and transferred at an optimal time when the uterine environment is prepared – especially with proper progesterone support.
Progesterone, often called the “pregnancy hormone,” prepares the endometrium (lining of the uterus) for implantation and supports early pregnancy.
Its levels at the time of transfer can significantly influence outcomes such as implantation, clinical pregnancy, and live birth rates.
This article explains what constitutes a “good” progesterone level for FET, how it’s measured, why it matters, how it’s managed, and how it fits into the broader IVF journey, including issues such as infertility symptoms, male infertility, semen analysis, ICSI treatment, and nutrition (foods for infertility).
Why Progesterone Matters in Frozen Embryo Transfer:
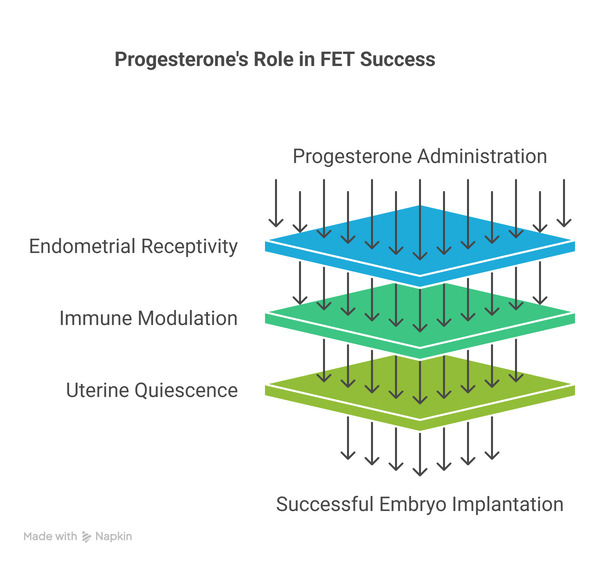
Progesterone is a steroid hormone produced by the corpus luteum after ovulation or administered externally in programmed FET cycles. Its key roles include:
- Endometrial receptivity: Progesterone transforms the estrogen-primed endometrial lining into a secretory phase favorable for embryo implantation.
- Immune modulation: Helps prevent embryo rejection.
- Uterine quiescence: Suppresses contractions for a stable environment.
In frozen cycles, especially programmed/medicated cycles, women receive exogenous progesterone via IVF injections, vaginal gels, or suppositories. Without a corpus luteum, external progesterone is required to mimic natural physiology.
What is a Good Progesterone Level for FET?
While no single value is universally agreed upon, research and clinical practice indicate the following:
Progesterone (serum) levels on the day of FET:
| Unit | Target Threshold | Notes |
|---|---|---|
| ng/mL | ≥10 ng/mL | Minimum generally associated with adequate implantation. |
| ng/mL | 10–20 ng/mL | Frequently cited “optimal clinical range.” |
| ng/mL | 20–30+ ng/mL | Some clinics aim here for higher pregnancy rates. |
| nmol/L | ≥50 nmol/L (~15.7 ng/mL) | Suggested minimum threshold in some studies. |
Summary of evidence:
- Many clinics consider ≥10 ng/mL as a minimum acceptable value.
- Higher levels (20–30 ng/mL) are often associated with better live birth rates.
- Extremely high serum values (>40 ng/mL) generally do not negatively impact outcomes.
Progesterone levels vary depending on the route of administration, timing relative to dosing, and type of FET protocol (natural vs. medicated).
Measuring Progesterone: When and How
Timing of measurement:
- One day before FET
- On the day of embryo transfer
Blood testing:
Serum progesterone is measured in ng/mL or nmol/L. 1 ng/mL ≈ 3.18 nmol/L.
Interpreting results:
Progesterone levels fluctuate depending on dosing; clinics standardize testing times post-dose to ensure consistency.
Progesterone Supplementation Protocols
Routes of supplementation:
- Vaginal progesterone: Suppositories or gels; local endometrial effect.
- Intramuscular progesterone in oil (PIO): Higher systemic levels; useful if serum levels are low.
- Combination therapy: Both vaginal and intramuscular routes for rapid increase in levels.
Timing:
Progesterone usually starts 3–5 days before blastocyst transfer and continues through the first trimester if pregnancy occurs.
Natural vs. Medicated FET Cycles:
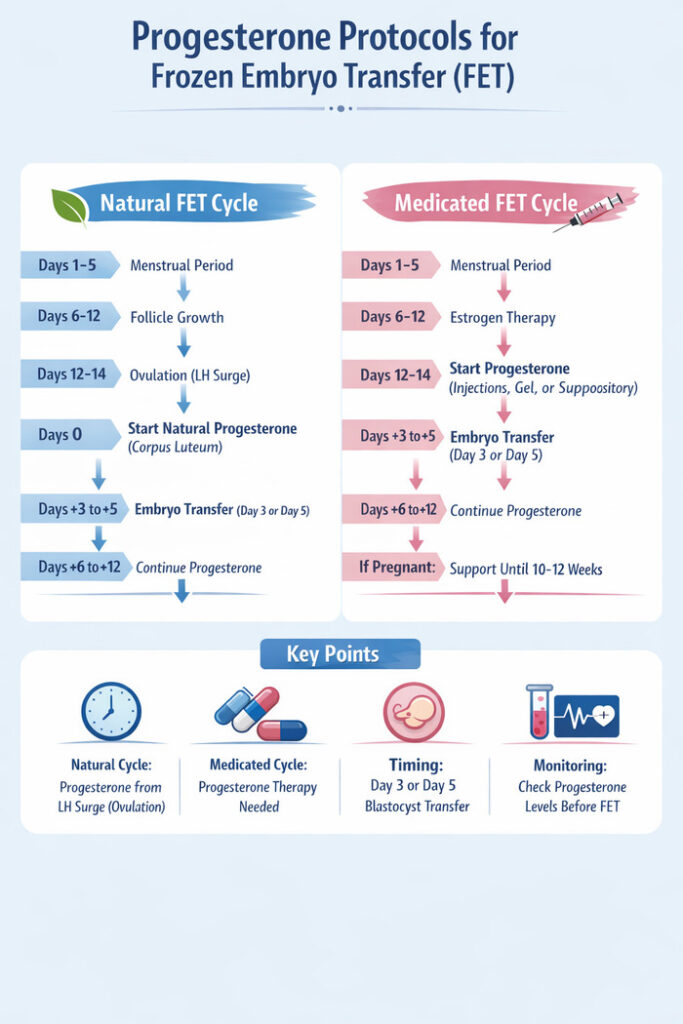
Here’s a printable guidance table comparing natural and medicated FET cycles:
| Feature | Natural FET Cycle | Medicated/Artificial FET Cycle |
|---|---|---|
| Ovulation | Monitored naturally | Suppressed; ovulation may not occur |
| Corpus luteum | Present; produces natural progesterone | Absent; progesterone provided exogenously |
| Progesterone start | After natural ovulation (LH surge) | After estrogen priming of endometrium |
| Monitoring | Ultrasound for follicle & endometrium | Ultrasound + blood tests for hormone levels |
| Pros | Fewer medications; natural hormone environment | Flexible scheduling; controlled endometrial thickness |
| Cons | Less predictable; cycle may cancel if ovulation missed | Higher medication load; cost |
| Recommended progesterone target | ≥10 ng/mL (from natural surge) | ≥10–20 ng/mL (from injections/supplements) |
Does Too Much Progesterone Harm FET Outcomes?
- Very high progesterone levels (>30–40 ng/mL) do not reduce implantation in medicated FET cycles.
- Clinics focus on individualized monitoring rather than rigid thresholds.
Integrating Progesterone Levels With Overall IVF Success:
1. Infertility symptoms: Irregular cycles, painful periods, ovulatory dysfunction, or unexplained infertility prompt fertility evaluation.
2. Semen analysis & Male infertility: Assessment of sperm count, motility, and morphology is critical. Male infertility contributes to nearly half of infertility cases, influencing decisions between IVF and ICSI treatment.
3. Unexplained infertility: FET with proper progesterone support can improve outcomes when embryos are available, even if previous testing is normal.
4. Nutrition: Foods for infertility like antioxidant-rich fruits, omega-3s, and low glycemic index foods support reproductive health, though diet alone cannot replace medical therapy.
Step-by-Step Progesterone Timeline for FET Cycles:
| Day | Natural FET Cycle | Medicated/Artificial FET Cycle | Notes |
|---|---|---|---|
| Day 1–5 | Menstrual bleeding starts | Menstrual bleeding starts | Cycle monitoring begins |
| Day 6–12 | Follicle development occurs naturally | Estrogen supplementation begins (oral/patch/injection) | Endometrium thickens to ≥7 mm |
| Day 12–14 | Ovulation detected via LH surge or ultrasound | Continue estrogen; suppress natural ovulation if needed | Progesterone not yet started |
| Day 0 (Ovulation / Progesterone start) | Natural ovulation occurs; corpus luteum produces progesterone | Start exogenous progesterone (IVF injections, vaginal gel, or suppository) | Timing of embryo transfer depends on embryo stage |
| Day +3 | Luteal phase supported naturally | Continue progesterone | Day 3 embryos can be transferred now |
| Day +5 | Luteal phase supported naturally | Continue progesterone | Blastocyst (Day 5) transfer possible |
| Day +6 to +12 | Progesterone continues naturally | Continue progesterone | Pregnancy test usually done 10–12 days after transfer |
| If pregnancy confirmed | Continue luteal support for 8–10 weeks | Continue progesterone until 10–12 weeks gestation | Progesterone supports early pregnancy |
Progesterone Levels and Live Birth Prediction:
| Study / Source | Progesterone Threshold | Outcome |
|---|---|---|
| Retrospective FET cohort | >20.6 ng/mL | Higher live birth and clinical pregnancy rates |
| Prospective cohort | ≥26.95 ng/mL | Optimized live birth prediction |
| Multicenter analysis | ≥50 nmol/L (~15.7 ng/mL) | Improved outcomes |
| Meta/Clinical practice | ≥10 ng/mL | Minimum threshold for adequate support |
Tips for Patients Undergoing FET:
Before transfer:
- Follow your clinic’s progesterone protocol
- Ask when and how your levels will be tested
- Expect IVF injections to be adjusted if needed
During transfer preparation:
- Ensure adequate estrogen and endometrial thickness (≥7–8 mm)
- Discuss timing of progesterone relative to embryo stage
Beyond progesterone:
- Explore free IVF treatment programs or insurance coverage
- Understand egg freezing cost if considering future fertility preservation
Conclusion:
Progesterone level is a critical biomarker in FET success. Evidence suggests:
- ≥10–15 ng/mL is generally acceptable
- 20–30+ ng/mL is often targeted for optimized outcomes
- Very high levels are generally safe in medicated cycles
Individualized monitoring by your IVF specialist ensures that progesterone supplementation and timing are optimized. Coupled with addressing male infertility, conducting semen analysis, using ICSI treatment when needed, and following supportive nutrition (foods for infertility), the chances of a successful FET cycle improve significantly.
FAQs:
A good progesterone level before FET is generally ≥10–15 ng/mL, with an optimal range around 20–30 ng/mL, which supports endometrial receptivity and implantation.
Progesterone prepares the uterine lining for embryo implantation and supports early pregnancy, making it a crucial factor in IVF treatment success.
Serum progesterone is measured via a blood test, usually one day before or on the day of embryo transfer, to ensure levels are sufficient for implantation.
Low progesterone can lead to a thin endometrium and reduced implantation rates, requiring adjustments via IVF injections or vaginal supplementation.
Very high progesterone levels rarely harm implantation in medicated FET cycles, but individualized monitoring ensures optimal hormonal support.
Healthy diet, exercise, and stress management may support natural hormone balance, but progesterone supplementation is crucial for successful IVF treatment.
Typically, levels are checked once before transfer, with follow-up if supplementation adjustments are needed to maintain optimal ranges.
While egg freezing cost is separate, women using stored eggs for FET still need proper progesterone monitoring to maximize implantation chances.
Progesterone is timed based on embryo stage: Day 3 embryos usually require 3 days of progesterone, while blastocyst (Day 5) transfer requires 5 days.

[…] Also Read: Good Progesterone Level for Frozen Embryo Transfer […]