IVF is a complex but life-changing treatment for couples struggling with infertility, whether due to male infertility, unexplained infertility, or other reproductive challenges.
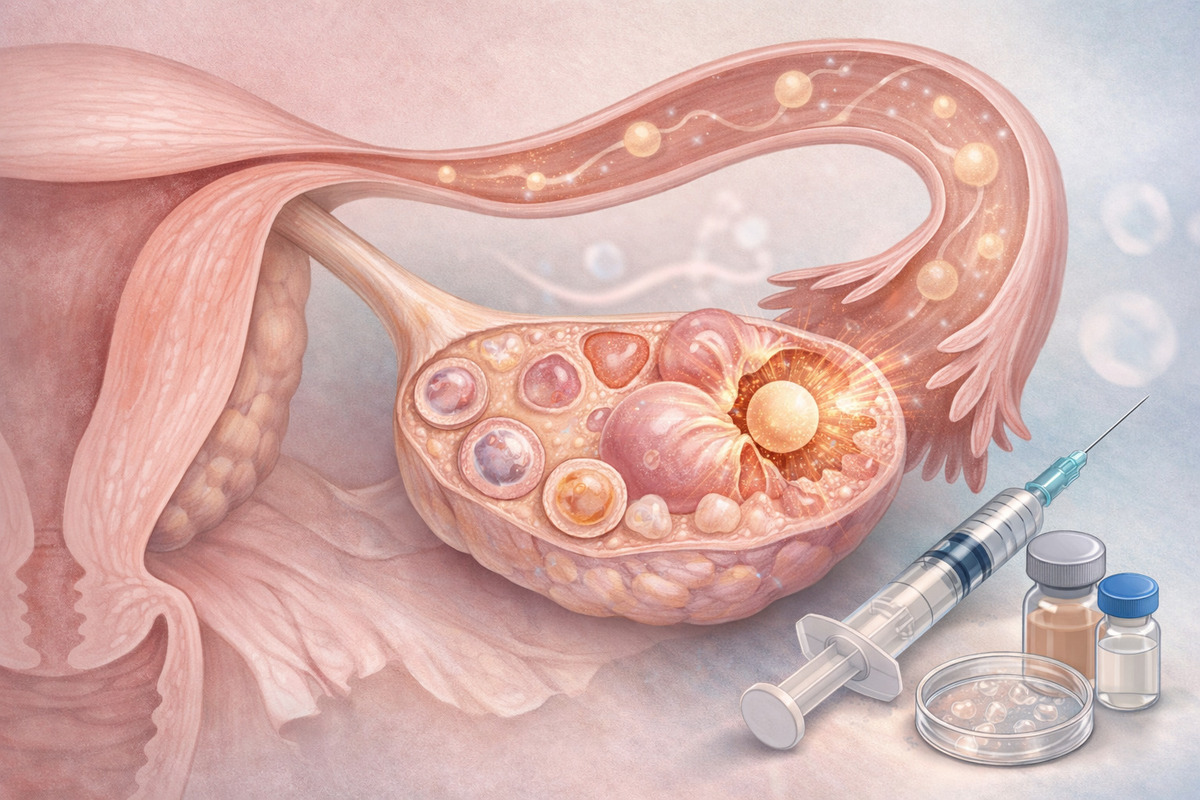
One of the most important steps in an IVF cycle is the trigger shot, which is carefully timed to ensure eggs are fully mature and ready for retrieval.
This timing is crucial because IVF success depends on collecting healthy eggs, fertilizing them in the lab, and transferring high-quality embryos back to the uterus. However, sometimes the body may ovulate naturally before the trigger shot, which can disrupt the entire IVF process.
Premature ovulation can lead to loss of eggs, reduced chances of fertilization, and even cycle cancellation, making it a stressful experience for couples who have already invested time, money, and hope into their IVF journey.
Couples undergoing IVF are often closely monitored through ultrasound scans, hormone tests, and semen analysis for male partners to track egg and sperm health, along with IVF injections that stimulate the ovaries.
The balance of hormones, the growth of ovarian follicles, and the precise timing of the trigger shot all work together to maximize the chances of a successful pregnancy.
In addition to medical supervision, lifestyle factors such as foods for infertility, balanced nutrition, and overall wellness can support reproductive health.
Even advanced procedures like ICSI treatment or egg freezing may come into play to preserve fertility or improve outcomes, with considerations like egg freezing cost or access to free IVF treatment programs for eligible couples.
Understanding what happens if ovulation occurs too early can help patients prepare, make informed decisions, and work closely with their fertility specialists to adjust their IVF plan, reduce risks, and improve the likelihood of a healthy pregnancy.
Understanding the Trigger Shot in IVF:
In conventional IVF protocols, the trigger shot typically contains a hormone such as human chorionic gonadotropin (hCG) or a GnRH agonist that mimics the body’s natural luteinizing hormone (LH) surge.
This surge promotes final maturation and prepares eggs for ovulation. In IVF, physicians schedule the trigger shot when ovarian follicles – fluid‑filled sacs containing eggs – reach an appropriate size (usually ~17–20 mm in diameter).
Once administered, ovulation usually occurs about 34–36 hours after the trigger shot – creating a predictable window for egg retrieval before natural ovulation releases the eggs into the body where they cannot be collected.
If ovulation happens before the trigger shot is administered, it can disrupt this carefully designed timing and affect several key aspects of IVF outcomes.
Why the Trigger Shot Timing Matters
The reason for precisely timing the trigger shot is simple:
- Premature ovulation means eggs are released into the fallopian tubes or peritoneal cavity where they cannot be retrieved by standard transvaginal aspiration.
- Without intact eggs to collect, embryologists cannot fertilize them via standard IVF or ICSI treatment in the lab.
- Mature eggs that are lost before retrieval mean fewer embryos and potentially lower pregnancy rates.
Table: Typical Ovulation & Trigger Timeline
| Event | Expected Timing |
|---|---|
| Follicle monitoring reaches threshold (~18–20 mm) | Begins IVF trigger planning |
| Trigger shot given | 0 hours |
| Most common ovulation window post‑trigger | ~34–36 hours |
| Latest potential ovulation post‑trigger | ~42 hours |
| Egg retrieval window scheduled | ~34–36 hours after trigger |
Source: Clinical timing used in IVF protocols
What Happens if You Ovulate Before Trigger Shot:
1. Loss of Eggs for Retrieval:
In IVF, premature ovulation means the follicles rupture before your egg retrieval procedure. Eggs released naturally are typically no longer retrievable by transvaginal aspiration, leading to a reduced egg count or even no eggs collected. This can directly lower your chances of fertilization and embryo development.
2. Cycle Cancellation:
If no eggs are available for retrieval, fertility specialists may cancel the cycle. A cycle cancellation means the medications, monitoring, and IVF injections up to that point may not result in a fresh embryo transfer or freeze. This can have clinical, psychological, and financial impacts, especially in settings where free IVF treatment programs or subsidized care limit the number of eligible cycles.
3. Lower Embryo Yield and Quality:
Even if some follicles remain and eggs are retrieved after premature ovulation, the number of eggs – and potentially their quality – may decline. Follicles that have started to rupture may yield eggs that are over‑mature or compromised, lowering the likelihood of fertilization effectiveness whether by standard IVF or ICSI treatment.
Why Early Ovulation Happens Despite Monitoring:
Premature ovulation can occur even with thorough monitoring due to several factors:
- Natural LH surge before medication suppression takes hold
- Inadequate suppression of natural ovulation despite antagonist or agonist protocols
- Rapid ovarian response, particularly in younger patients or those with PCOS
- Missed or late trigger shot timing due to scheduling or compliance issues
Fertility clinics use frequent ultrasounds and hormone tests to reduce this risk – but variability in individual responses can still lead to early ovulation.
Ovulating Before Trigger:
Cycle cancellation or a low egg count after premature ovulation can be an emotional blow. Patients often report feelings of disappointment and stress – especially after months of daily injections, ultrasounds, and emotional investment.
For couples navigating male infertility or issues like low sperm count diagnosed via semen analysis, this added setback can feel particularly tough on the journey to parenthood.
Your fertility care team can help by offering counseling resources and planning adjustments for future cycles.
How Fertility Clinics Minimize the Risk:
Fertility experts use several strategies to prevent premature ovulation:
1. Tailored Medication Protocols:
Clinics prescribe gonadotropin-releasing hormone (GnRH) antagonists or agonists alongside stimulation drugs to prevent the body’s own LH surge. Adjusting protocols based on your response helps lower the risk of early ovulation.
2. Close Monitoring:
Frequent ultrasounds and hormone testing have patients in the clinic about every 1–2 days during the follicular phase. If a sudden LH rise is detected, protocols may be adjusted in real time.
3. Adjusted Trigger Timing:
In some cases, if follicles are maturing faster than anticipated, clinicians may decide to trigger earlier than standard thresholds to avoid premature LH surges.
Nutrition and Lifestyle:
Although scientific evidence on nutrition influencing ovulation timing is limited, adopting supportive dietary habits can optimize overall reproductive health. Research and clinical practice often suggest including foods for infertility that promote balanced hormones and metabolic health, such as:
- Healthy fats (avocados, nuts)
- Lean proteins and omega‑3 sources (fish, legumes)
- Whole grains and fiber to support insulin balance
While diet alone cannot prevent premature ovulation, healthy nutrition contributes to a stable endocrine environment that supports your IVF injections and ovulatory control.
Conclusion:
Early ovulation before a trigger shot is a frustrating and sometimes unavoidable event in IVF cycles.
It can lead to loss of eggs, cycle cancellation, and emotional hardship. However, with vigilant monitoring, personalized protocols, and collaborative care with your fertility specialist, the risk can be minimized.
Successful IVF requires both scientific precision and patient resilience. Understanding how and why premature ovulation occurs helps you make informed choices – for example, adjusting stimulation strategies, considering egg freezing cost and alternatives, or blending protocols like ICSI treatment to maximize every chance of success.
If you’re experiencing challenges or concerns about your stimulation cycle or timing of trigger shots, your reproductive endocrinologist is your primary resource.
They can interpret your infertility symptoms and labs – whether it’s unexplained infertility or specific male factors diagnosed via semen analysis – and tailor your IVF journey for the best possible outcome.
FAQs:
Premature ovulation can cause loss of eggs, reduce embryo yield, and may lead to cycle cancellation in your IVF treatment. It affects both standard IVF and ICSI procedures.
Yes, if ovulation occurs before the trigger shot, eggs may be released naturally and become unretrievable, lowering the chances of successful fertilization.
Early ovulation reduces the number of eggs collected, which can affect embryo quality and overall pregnancy chances in IVF or ICSI treatment cycles.
Carefully timed IVF injections and hormone protocols help control follicle maturation, but some patients may still experience early LH surges causing ovulation.
Male infertility diagnosed via semen analysis can compound IVF challenges, and early ovulation may further reduce egg-sperm fertilization opportunities.
ICSI treatment may still be possible if some eggs are retrieved, but early ovulation can limit the number of mature eggs available for injection.
Clinics use frequent ultrasounds and hormone tests to track follicle growth and prevent early ovulation, ensuring IVF injections and trigger shots are timed accurately.
Lifestyle factors like proper diet, including foods for infertility, stress management, and healthy routines may support hormone balance but cannot fully prevent early ovulation.
[…] Also Read: What Happens if You Ovulate Before Trigger Shot […]